Sleep Paralysis and Terrifying Hallucinations: Understanding the Experience
During sleep paralysis, you'll find yourself conscious but unable to move as your body remains in its natural sleep-induced paralysis state. You might experience terrifying hallucinations like shadowy figures, pressure on your chest, or a menacing presence in the room - affecting up to 75% of cases. While these episodes typically last seconds to minutes, they can feel much longer and deeply disturbing. You're not alone, as about 8% of people experience this phenomenon at least once. Understanding the science behind sleep paralysis, along with proven coping strategies, can help you traverse this unsettling but manageable condition.
What Is Sleep Paralysis
Lying motionless in bed while fully awake, unable to move a muscle or cry out for help - this is the unsettling reality of sleep paralysis. During these episodes, you'll find yourself completely conscious but temporarily paralyzed, trapped in a state between wakefulness and sleep. Your mind is alert, but your body won't respond to any commands.
Sleep paralysis occurs when there's a disconnect between your brain and body during the shift to or from REM sleep. While experiencing this condition, you might encounter vivid hallucinations, often involving a threatening presence in your room. These hallucinations can make an already frightening experience even more terrifying.
You're not alone if you've faced this sleep disorder - approximately 8% of people will experience sleep paralysis at least once in their lifetime. While there's no guaranteed way to prevent episodes entirely, maintaining good sleep hygiene can help reduce their frequency. If you're experiencing frequent episodes that interfere with your daily life, it's important to consult a medical professional who can evaluate your condition and recommend appropriate treatments or lifestyle changes to manage this unsettling phenomenon.
Common Sleep Paralysis Hallucinations
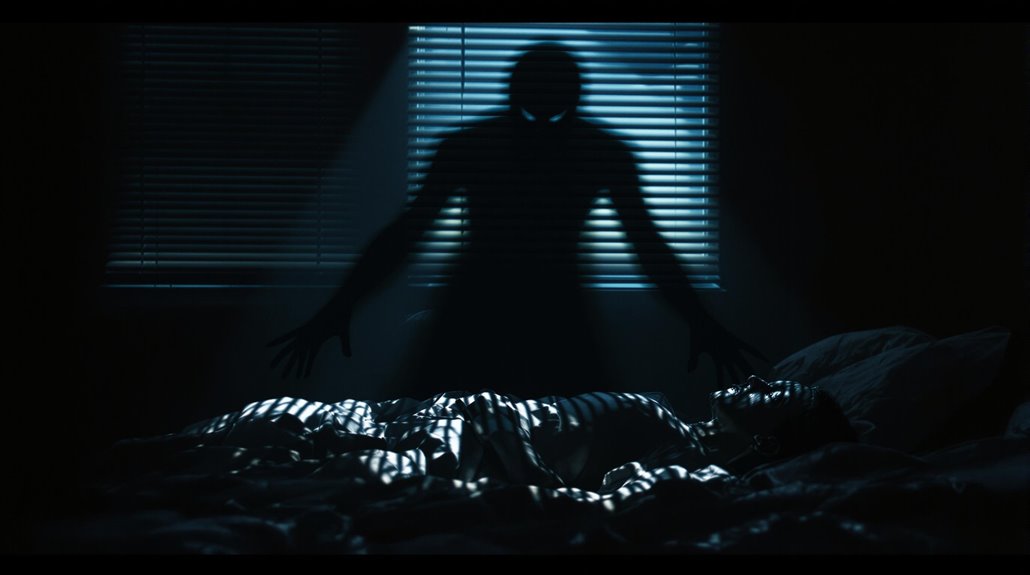
While sleep paralysis itself can be frightening, the hallucinations that often accompany these episodes can intensify the terror. You might experience vivid and disturbing sensations during these episodes, with up to 75% of cases involving some form of hallucination. These experiences often occur during the shift between REM sleep and wakefulness, when your mind is conscious but your body remains in its paralyzed state.
The most common types of sleep paralysis hallucinations include:
- A menacing presence or shadowy figure watching you from within the room
- An incubus or heavy weight pressing down on your chest, creating a sensation of suffocation
- Floating sensations or out-of-body experiences that feel incredibly real
These hallucinations can profoundly impact your sleep quality and overall well-being. You might feel helpless as you experience these terrifying visions, unable to move or call for help. While approximately 20% of people encounter these episodes occasionally, understanding that they're a natural phenomenon can help reduce anxiety. If you're experiencing frequent sleep paralysis with hallucinations, consider evaluating your sleep hygiene and consulting a healthcare provider, as conditions like sleep apnea can increase their likelihood.
Medical Causes and Risk Factors

Sleep paralysis's underlying causes stem from a complex interplay of medical conditions, lifestyle factors, and genetic predispositions. Your risk of experiencing sleep paralysis increases substantially if you have irregular sleep habits or suffer from sleep deprivation. Medical conditions like narcolepsy can disrupt your REM sleep cycle, making you more susceptible to these unsettling episodes.
Your genetics might predispose you to sleep paralysis, as research shows it often runs in families and relates to specific variations in sleep-wake cycle genes. If you're dealing with mental health challenges like anxiety, depression, or PTSD, you're more likely to encounter frequent episodes of sleep paralysis and its accompanying hallucinations. Even your sleeping position matters - lying on your back increases your chances of experiencing these episodes.
The key risk factors you should be aware of include:
- Disrupted sleep schedules
- Chronic sleep deprivation
- Existing medical conditions affecting sleep
- Family history of sleep paralysis
- Mental health conditions
- High stress levels
- Back sleeping position
Understanding these risk factors can help you identify and potentially modify behaviors that contribute to sleep paralysis episodes.
Cultural Interpretations Through History
Beyond the medical explanations we now understand, cultures worldwide have long sought to make sense of sleep paralysis through their own distinct interpretations. While we are aware, sleep paralysis occurs during rapid eye movement (REM) sleep, ancient cultures developed fascinating explanations for these terrifying experiences.
Japanese folklore describes "kanashibari," where victims feel bound by invisible silkworms, explaining the paralysis you experience during REM sleep. Newfoundland's "Old Hag" phenomenon depicts a supernatural being that sits on your chest, matching the pressure sensations common during sleep paralysis episodes. Hmong culture attributes hallucinations during sleep paralysis to visits from evil witches, connecting supernatural beliefs to the frightening incubus hallucinations many report.
Sleep paralysis is more common than you might think, and these cultural interpretations show how humans have tried to explain this mysterious phenomenon throughout history. While sleep paralysis without scientific understanding led to supernatural explanations, these shared experiences across cultures reveal striking similarities in how people describe their encounters. From demonic presences to night hags, these interpretations reflect the universal human need to understand the terrifying hallucinations often accompanying sleep paralysis.
Breaking Free During Episodes

During an episode of sleep paralysis, staying calm is your most powerful tool for breaking free. When you find yourself unable to move and experiencing temporary paralysis, remember that the episode will pass. While you cannot move most of your body, focus on making small movements with your fingers and toes, as these are often the first parts to regain mobility.
If you're experiencing recurrent isolated sleep paralysis, try shifting your attention to your other senses. Listen to ambient sounds or focus on the feeling of your bedsheets against your skin. While you might feel the urge to struggle, this can actually prolong the episode. Instead, concentrate on controlling your breathing with slow, deliberate breaths. If possible, try to move your eye muscles or attempt to call out for help, as these actions can sometimes interrupt the paralysis.
To prevent sleep paralysis episodes, remind yourself that while frightening, these experiences aren't harmful. When you feel trapped and powerless, focusing on this fact can help reduce anxiety. Remember, the temporary nature of sleep paralysis means relief is always just moments away.
Prevention and Management Strategies
Effective prevention strategies can greatly reduce the frequency and severity of sleep paralysis episodes. If you're experiencing recurring episodes, maintaining good sleep hygiene and a consistent sleep schedule should be your first line of defense. You'll want to establish regular sleep patterns while avoiding caffeine and alcohol before bedtime.
- Keep a sleep diary to track your episodes and identify potential triggers
- Practice relaxation techniques like deep breathing and meditation before bed
- Consult a sleep specialist if episodes persist or cause significant distress
You can further manage your symptoms by incorporating relaxation techniques into your daily routine. These methods, combined with cognitive-behavioral therapy, can help you address the underlying anxiety and fear associated with sleep paralysis. If you're still struggling, don't hesitate to discuss medication options with your healthcare provider, as antidepressants or benzodiazepines may help in some cases.
Scientific Research and Studies

Recent scientific research has unearthed fascinating revelations into the neurological mechanisms behind sleep paralysis. Scientists have found that your brain gets caught between REM sleep and wakefulness during these episodes, creating a unique state where you're conscious but unable to move. Brain imaging studies have revealed heightened activity in areas responsible for self-awareness and threat detection, helping explain why you might feel intensely alert during these experiences.
Research shows that sleep deprivation and irregular sleep patterns considerably increase your risk of experiencing sleep paralysis. If you're dealing with conditions like narcolepsy, PTSD, or anxiety, you're also more likely to encounter these episodes. What's particularly intriguing is that up to 75% of cases involve hallucinations, where you might sense an intruder or experience complex sensory phenomena.
While medical treatment research remains limited, scientists have identified several effective management approaches. You'll find that maintaining consistent sleep schedules and practicing relaxation techniques can help reduce both the frequency and intensity of episodes. Current research continues to focus on understanding brain activity patterns during sleep paralysis to develop more targeted interventions for those affected by this phenomenon.
Physical and Emotional Effects
The physical and emotional toll of sleep paralysis can be overwhelming for those who experience it. When sleep paralysis occurs, you'll find yourself unable to move or speak, often accompanied by a crushing sensation on your chest. If you suffer from sleep paralysis, you're likely to experience intense fear and panic during these episodes, which can cause emotional distress long after the event has passed.
- Your body remains completely immobilized while your mind is fully conscious
- You may feel intense pressure on your chest, making breathing feel difficult
- You might experience vivid, terrifying hallucinations that feel extremely real
Understanding sleep paralysis is pivotal because up to 75% of these episodes include hallucinations involve sensing a threatening presence in the room. While it's significant to observe that sleep paralysis is more common than you might think, the psychological impact can be severe. Most people who experience sleep paralysis describe it as terrifying, leaving them feeling helpless and shocked. Though the cause of sleep paralysis isn't always clear, the emotional aftermath can persist, leading to anxiety about future episodes. Curiously, while most experiences are frightening, a small number of people report more benign or even comforting hallucinations during their episodes.
Sleep Disorders and Connections

Beyond its standalone occurrence, sleep paralysis often intertwines with various other sleep disorders and mental health conditions. If you're experiencing sleep paralysis, you might also be dealing with conditions like obstructive sleep apnea or narcolepsy, where your brain's ability to regulate sleep cycles becomes disrupted. Deep Sleep patterns can be particularly affected when these conditions overlap.
Research in sleep medicine has shown that people with sleep paralysis frequently struggle with post-traumatic stress disorder (PTSD), anxiety, or bipolar disorder. Your risk increases dramatically if you maintain irregular sleep patterns, whether due to shift work, jet lag, or poor sleep habits. The condition is often characterized by a complex interplay of genetic and environmental factors, as studies on twins have revealed.
You'll want to pay attention to your lifestyle choices, as certain behaviors can trigger episodes. Using alcohol before bed, taking specific medications, or experiencing chronic sleep deprivation can all increase your likelihood of experiencing sleep paralysis. Understanding these connections helps healthcare providers develop more effective treatment strategies customized to your specific situation.
Treatment Options and Support
When facing sleep paralysis, effective treatment often kicks off with a thorough evaluation by a sleep specialist to determine the best approach for your situation. A medical expert can help identify if your episodes stem from underlying conditions like PTSD or poor sleep habits that disrupt your natural REM atonia cycle.
- Cognitive behavioral therapy (CBT) helps you manage anxiety and fear associated with episodes through proven psychological techniques
- Medications like antidepressants or benzodiazepines may be prescribed if you experience severe or frequent episodes
- Support groups connect you with others who understand your experience and share coping methods
Your treatment plan will likely include improving sleep hygiene through consistent bedtime routines and relaxation techniques. This might involve setting regular sleep schedules, creating a calm bedroom environment, and practicing stress-reduction methods before bed. Many people find that joining support groups, either in-person or online, provides helpful emotional relief and practical advice. You'll learn that you're not alone in your experiences, and you can benefit from others' perspectives into managing episodes. Remember that while sleep paralysis can be frightening, various treatment options and support systems are available to help you cope effectively.




